Abstract
Introduction: The randomized phase 3 ENDEAVOR trial demonstrated superior progression-free survival (PFS), overall survival (OS), and health-related quality of life in patients with relapsed or refractory multiple myeloma (RRMM) for patients treated with carfilzomib (56 mg/m2) and dexamethasone (Kd56) compared with bortezomib and dexamethasone (Vd). In patients with relapsed MM, the time of therapy initiation might impact treatment outcome. Prior studies have demonstrated a median of 5 months between the presence of biochemical and symptomatic relapse (Lopez. Leuk Res Rep. 2015;4:64-69). Herein, we report a post hoc subgroup analysis from the ENDEAVOR study to evaluate the impact of initiating Kd56 therapy upon biochemical relapse.
Methods: Adults with RRMM who previously received 1-3 lines of therapy and had measurable disease were eligible to participate in the ENDEAVOR trial. Symptomatic disease was not required for eligibility. Kd56 patients received carfilzomib on days 1, 2, 8, 9, 15, and 16 as a 30-minute intravenous infusion and dexamethasone (20 mg) on days 1, 2, 8, 9, 15, 16, 22, and 23 of a 28-day cycle. Vd patients received bortezomib (1.3 mg/m2; intravenous bolus or subcutaneous injection) on days 1, 4, 8 and 11 and dexamethasone (20 mg) on days 1, 2, 4, 5, 8, 9, 11, and 12 of a 21-day cycle. Treatment continued until disease progression, physician decision, unacceptable toxicity, withdrawal of consent, or death. This post hoc subgroup analysis evaluated PFS, OS, and safety in subgroups defined according to the presence of symptoms at the time of enrollment. Patients with RRMM who experienced biochemical progression without CRAB symptoms (hypercalcemia, renal impairment, anemia, or bone lesions) upon relapse were considered asymptomatic, whereas symptomatic patients were those who had CRAB symptoms upon relapse. In each subgroup, PFS and OS were compared between treatment arms using an unstratified Cox proportional hazards model.
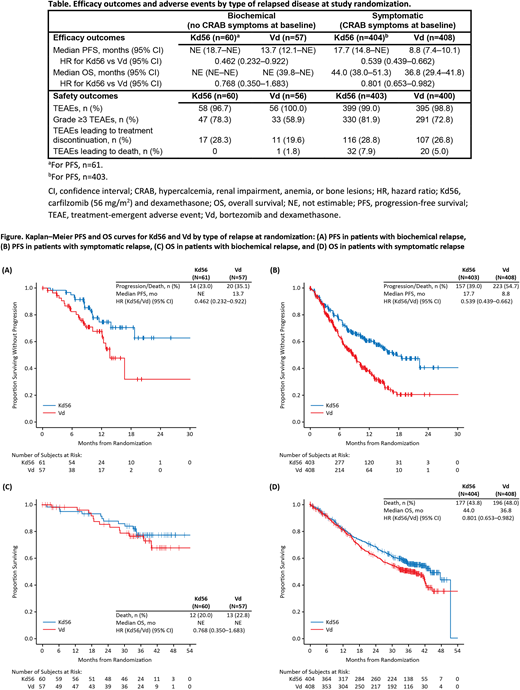
Results: Of the 929 patients enrolled and randomized in ENDEAVOR, 117 (12.6%) were asymptomatic (Kd56, n=60; Vd, n=57) and 812 (87.4%) were symptomatic (Kd56, n=404; Vd, n=408). In the asymptomatic group, the median PFS was not estimable (NE) for Kd56 vs 13.7 months for Vd (hazard ratio [HR]: 0.462; 95% confidence interval [CI]: 0.232-0.922), and the median OS was NE for either treatment arm (HR: 0.768; 95% CI: 0.350-1.683) (Table). In the symptomatic group, median PFS was 17.7 months for Kd56 vs 8.8 months for Vd (HR: 0.539; 95% CI: 0.439-0.662), and median OS was 44.0 months for Kd56 vs. 36.8 months for Vd (HR: 0.801; 95% CI: 0.653-0.982) (Table). Kaplan-Meier PFS and OS curves are shown in the Figure. The rate of grade ≥3 treatment-emergent adverse events (Kd56 vs Vd) was 78.3% vs 58.9% in the asymptomatic group and 81.9% vs 72.8% in the symptomatic group (Table).
Conclusions: Kd56 demonstrated superior survival outcomes compared with Vd in patients with RRMM, regardless of presence of CRAB symptoms at study randomization. As expected, outcomes were improved when Kd56 was initiated early in the disease course, before CRAB symptoms occurred. The small size of the subgroups in this study is a limitation. However, the findings warrant further investigation. The safety profile of Kd56 in both subgroups was consistent with that in the overall population as previously reported (Dimopoulos. Lancet Oncol. 2016;17:27-38; Siegel, Clin Lymphoma Myeloma Leuk. 2017;17:e142). Overall, Kd56 had a favorable benefit-risk profile in both patients with biochemical and symptomatic relapse.
Moreau:Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees. Siegel:Merck: Consultancy, Honoraria, Speakers Bureau; Amgen: Consultancy, Honoraria, Speakers Bureau; Celgene: Consultancy, Honoraria, Research Funding, Speakers Bureau; Novartis: Honoraria, Speakers Bureau; BMS: Consultancy, Honoraria, Speakers Bureau; Karyopharm: Consultancy, Honoraria; Takeda: Consultancy, Honoraria, Speakers Bureau; Janssen: Consultancy, Honoraria, Speakers Bureau. Goldschmidt:Janssen: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Research Funding; Sanofi: Consultancy, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; ArtTempi: Honoraria; Novartis: Honoraria, Research Funding; Bristol Myers Squibb: Consultancy, Honoraria, Research Funding; Chugai: Honoraria, Research Funding; Mundipharma: Research Funding; Adaptive Biotechnology: Consultancy; Amgen: Consultancy, Research Funding. Niesvizky:Takeda: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Amgen Inc.: Consultancy, Research Funding; Janssen: Consultancy, Research Funding. Bringhen:Takeda: Consultancy; Janssen: Honoraria, Other: Advisory Board; Amgen: Honoraria, Other: Advisory Board; Celgene: Honoraria; Bristol-Myers Squibb: Honoraria. Orlowski:Spectrum Pharma: Research Funding; BioTheryX: Research Funding; Amgen: Consultancy, Research Funding; Takeda: Consultancy; Sanofi-Aventis: Consultancy; Janssen: Consultancy; Bristol-Myers Squibb: Consultancy; Celgene: Consultancy; Kite Pharma: Consultancy. Blaedel:Amgen: Employment, Equity Ownership. Yang:Amgen Inc.: Employment, Equity Ownership. Dimopoulos:Takeda: Honoraria; Janssen: Honoraria; Celgene: Honoraria; Bristol-Myers Squibb: Honoraria; Amgen: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal